Experience of laparoscopic drainage of posttraumatic intramural hematomas of duodenum in children
Yury Yu. Sokolov 1, Sergey V. Stonogin 2, Grachik T. Tumanyan 1, Israil Sad. Allakhverdiyev 1, Anna N. Shapkina 4
Experience of laparoscopic drainage of posttraumatic intramural hematomas of duodenum in children
[1] Russian Medical Academy of Continuous Professional Education, Moscow
[2] Сhildren's city hospital of Z.A. Bashlyaeva, Moscow
[3] Detskaya gorodskaya bolnitsa svyatogo Vladimira, Moscow
[4] Pacific State Medical University, Vladivostok
Abstract.
Objective. Demonstrate the possibility of minimally invasive laparoscopic interventions in children with traumatic duodenal injuries.
The diagnosis and treatment of traumatic injuries of the duodenum is one of the most complex and rather controversial sections of surgery. To date, the incidence of duodenal damage in the structure of all injuries of the abdominal cavity is only 1.2% [1].
Materials and methods. The article presents 2 clinical observations of post-traumatic intramural duodenal hematoma in children who underwent minimally invasive laparoscopic interventions.
Results. Treatment of post-traumatic hematoma of the duodenum using minimally invasive surgical interventions in children is possible and highly effective.
Summary. Post-traumatic hematoma of the duodenum is treated with the use of minimally invasive surgical interventions, phenomena of high intestinal obstruction are stopped in a short time, early enteral nutrition begins, the patient is energised in the early stages.
Keywords:
laparoscopy, duodenal injury, intramural hematoma, children.
Diagnosis and treatment of traumatic injuries of the duodenum is one of the complex and rather controversial sections of surgery. To date, the incidence of duodenal damages in the structure of all injuries of the abdominal cavity is only 1.2% [1].
The article presents 2 clinical observations of post-traumatic intramural duodenal hematoma in children who underwent minimally invasive laparoscopic interventions.
Clinical case No. 1
Girl “S” 8y.o. Complained of abdominal pain and repeated vomiting. The patient’s medical history showed that two weeks before admission she hit her stomach on the metal side of a swimming pool.
The general state is moderately severe. A gastric tube was installed - up to 200 ml of stagnant discharge was excreted. The skin cover is normally coloured, with no rash. Intact oral pharynx. Vesicular breathing in all lung sections, without any wheezing. The abdomen is not distended, soft, painful on palpation in the right hypochondrium. Negative symptoms of peritoneal irritation. Normal stool after an enema, without dysuria. Both common blood count and blood chemistry showed no deviations.
Ultrasound of the abdominal organs: in the subhepatic space projection, a mass lesion of 7 x 4 cm is detected on the right. Conclusion: pancreatic head cyst? Hematoma? Lymphangioma? (Fig. 1)

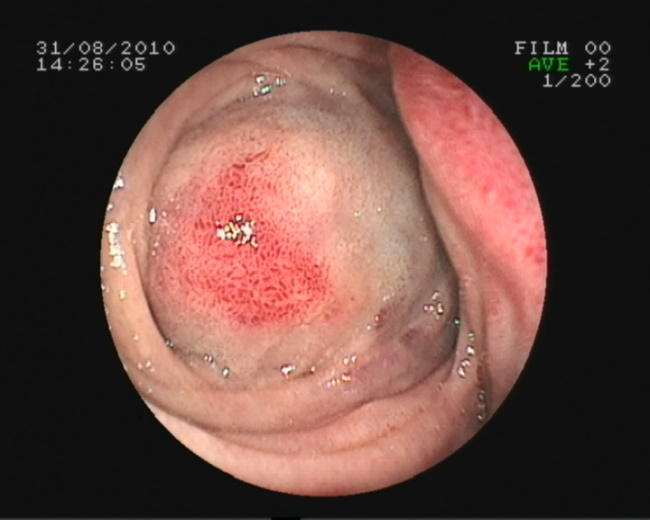
The endoscopy showed the lumen of the descending branch of the duodenum blocked from the outside, the mucosa with petechial hemorrhages (Fig. 2).
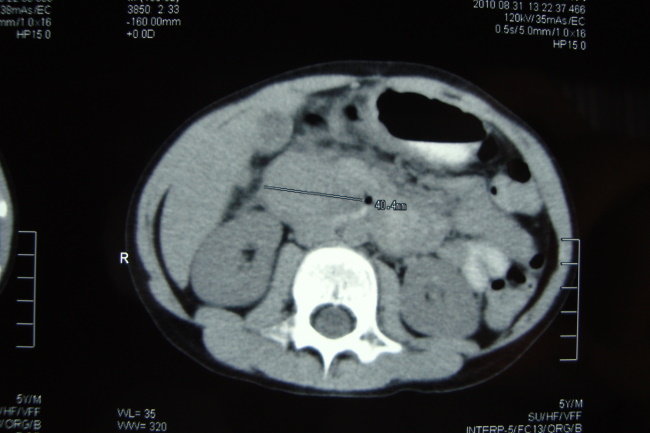
The spiral computed tomography of the upper gastrointestinal tract with contrast enhancement revealed an obstacle at the level of the descending branch of the duodenum (Fig. 3).
Partial high bowel obstruction was diagnosed. The phenomena of partial high bowel obstruction cause urgent indications for surgical treatment. Conclusion - compression of the duodenum by a mass lesion.
A laparoscopy was performed, which found blood imbibition of subperitoneal tissue. There is a small amount of serous-hemorrhagic effusion in the pelvis. The posterior abdominal layer along the descending part of the duodenum is dissected. After mobilisation of the duodenum according to Kocher’s method, the intramural duodenal hematoma in the descending branch was visualised. A longitudinal rupture of the serous-muscular layer of the intestine over 2 cm was revealed, while maintaining the integrity of the mucous membrane. Under pressure, up to 100 ml of dark liquid blood was released (Fig. 4).
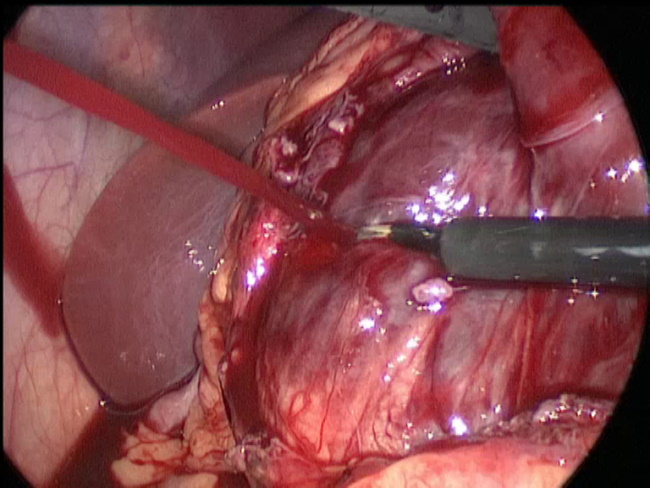
The intestinal wall defect was closed with three intracorporeal nodal sutures with 3–5 Vicryl thread. During the control intraoperative esophagogastroduodenoscopy, a slight deformation of the lumen wass visualised in the upper part of the descending branch of the duodenum. Under the endoscopic guidance, a nasogastric neural probe was performed. The abdominal cavity is dried, drained through the right trocar opening with a tubular drainage into the subhepatic space. Conclusion: an extensive intramural hematoma of the descending branch of the duodenum. Partial high bowel obstruction.
The postoperative course without any complications. Antibacterial therapy, infusion therapy, and parenteral nutrition were performed.
Drainage from the subhepatic space was removed on day 5. On day 6 after the operation, the probes were removed from the stomach and duodenum, enteral feeding was started. Against the background of the treatment, the condition of the child was improving. The patient had no complaints. Enteral nutrition was assimilated. No fever observed. The abdomen is soft, deeply palpable in all sections, painless. Normal stool. A follow-up ultrasound of the abdominal organs revealed no pathology. The wounds healed by primary intention. The patient was discharged in satisfactory condition.
Clinical case No. 2
Boy “G” 6y.o., was urgently hospitalised with suspected acute appendicitis with complaints of intense abdominal pain, repeated vomiting, and low-grade fever. The ultrasound of the abdominal cavity in the epigastrium, in the projection of the pancreatic head, duodenum, and portal of the liver presumably retroperitoneally visualised a rounded circular mass with fuzzy, even contours of the cystic type with heterogeneous content (fine suspension + echodense inclusions), 8.0 x 4.0 x 4.0 cm. (hematoma? Cyst of the head of the pancreas? Lymphangioma?). The patient underwent abdominal R-graphy which revealed a sharply reduced intestinal gas filling. Infusion therapy was started (salt solutions, saline, glucose 10%). The condition of the child worsened, abdominal pain intensified and repeated vomiting was noted.
The boy had indications for diagnostic laparoscopy, which revealed a large cystic mass (up to 10 cm in diameter) located retroperitoneally in the projection of the omental bursa. A cyst puncture was performed, about 30 ml of serous-hemorrhagic content was removed, after which the tension of the mass slightly decreased. A safety drainage was installed in the small pelvis through a trocar incision in the left epigastric region.
After the laparoscopy on day 2, an MRI was performed that revealed a mass retroperitoneal pathological lesion. A follow-up ultrasound found echoes of a cystic formation of retroperitoneal space, possibly coming from the head of the pancreas. A suspected impaired passage at the level of the pyloric stomach.
Given the results of the examinations, the presence of signs of high partial intestinal obstruction was the indication for relaparoscopy and revision of the abdominal cavity. Relaparoscopy in the projection of the horseshoe of the duodenum and the pancreatic head in the retroperitoneal space revealed a large mass lesion that displaces the preceding organs. When displacing the transverse colon upward in the retroperitoneal space to the right of the descending branch of the duodenum, the intense cystic mass of cyanotic colour is determined. The posterior abdominal layer over the mass lesion was dissected - up to 500 ml of liquid blood and clots were removed under pressure. The revision found an intramural hematoma of the descending and lower horizontal sections of the duodenum with exfoliation of the serosa over a large extent. A further revision of the cavity found that the posterior part of hematoma was presented to the anterior wall of the inferior vena cava. It was not possible to establish the source of the bleeding because it had stopped. The abdominal cavity was dried, drained by tubular drainage in the cavity of the opened hematoma through the right trocar access. Conclusion: Tense massive intramural hematoma of the duodenum.
The postoperative course was satisfactory. The child received antibacterial, hemostatic treatment. Against the background of the treatment, the child's condition improved. The pain subsided. During the follow-up ultrasound of the abdominal organs on day 5 after the operation, no findings were obtained for cystic formation. Drainage from the hematoma cavity was removed on day 6 after surgery. Primary wound healing. The boy was discharged in a satisfactory condition.
Discussion
The incidence of intramural post-traumatic hematomas of the duodenum in children is 2% [2]. Among the patients, 70% are boys whose average age is 8 years (from 3 months to 16 years) [3]. The frequency of complications and the mortality rate in such victims are high and range from 30 to 100% [4]. This is explained by the presence of multiple injuries of the abdominal organs, the features of the anatomy of the duodenum (the serous membrane does not completely cover the duodenum and cannot prevent the spread of hematoma), possible serious complications (duodenal fistula, retroperitoneal phlegmon, peritonitis, pancreatic necrosis, intestinal suture failure sepsis, progressive exhaustion).
Among the mechanisms of traumatic damage to the duodenum in children are a direct blow to the epigastrium, a car injury, an injury to caused by a bicycle wheel, falls, being kicked by a horse, mistreatment of a child, and iatrogenic injuries during endoscopic biopsy [5], [7], [8]. The first report of intramural hematoma of the duodenum of subserous localisation belongs to Mc. Lauchlan, who in 1838 described the “blood masses” of the duodenal wall in a patient with an abdominal trauma [9]. In pediatric practice, information about similar injuries of the duodenum is very scarce. According to I.N. Grigovich [10], who summarised information about 102 closed injuries of the duodenum in children, 72 cases were an intramural hematoma, in 30 cases there was a rupture of the duodenum, 5 children from the group with a duodenal rupture died. G. Tsuman et al. [11] provide information on 6 children aged 4 to 12 years with isolated damage to the retroperitoneal part of the duodenum. One child had an extensive intramural hematoma that caused high intestinal obstruction, another child had a complete circular rupture of the 12 duodenum, and the remaining 4 children had a partial rupture at the level of the lower horizontal part.
Damage to the duodenum is difficult to diagnose not only before surgery, but also during a laparotomy [12],[13],[14]. The most common symptoms are abdominal pain, nausea, and vomiting [15]. During examination, the key signs are the tension of the muscles of the abdominal wall, pain during palpation in the epigastrium, and hematomas in the epigastric region.
The most informative methods for diagnosing this pathology are ultrasound, X-ray with barium, and spiral computed tomography with contrast enhancement, to determine the location, size of the retroperitoneal hematoma, as well as assess the condition of the pancreas and neighbouring organs [6], [14].
According to literature, more often, isolated damage to the duodenum with the formation of an intramural hematoma can be treated conservatively (nasogastric intubation, complete parenteral nutrition for 2 weeks) but it can take 3 weeks of therapy to achieve a clinical effect. The duodenum is very well supplied with blood, which contributes to the rapid resorption of the hematoma and serves as a prevention of cicatricial stenosis [7], [15], [16]. Indications for surgical treatment can be a rapid increase in the volume of hematoma, perforation of the duodenum, and the ineffectiveness of conservative treatment.
Successful percutaneous hematoma drainage under ultrasound guidance has been described in two boys aged 12 and 14 years [16]. After installing the drainage according to this technique, the patients began to receive nutrition on the 1st day orally with the disappearance of signs of pyloric obstruction and the absence of signs of pancreatitis; on day 4-12, the drainage was removed.
The available literature describes one successful case of treatment of the duodenal hematoma using laparoscopic access [2].
Thus, the clinical observations presented by us demonstrate the possibility of treating the post-traumatic hematoma of the duodenum using minimally invasive surgical interventions, which can quickly stop high bowel obstruction, start early enteral nutrition, and energise the patient in the early stages [16].
References
1. Chirkov R.N., Abakumov M.M., Blokhin V.N. Diagnosis and surgical tactics for traumatic intramural duodenal hematomas // 2008. N. 5. P. 33–36
2. Banieghbal B, Vermaak C, Beale P: Laparoscopic drainage of a posttraumatic intramural duodenal hematoma in a child. J Laparoendosc Adv Surg Tech A. 18(3):469-72, 2008
3. Gutierrez IM, Mooney DP. Operative blunt duodenal injury in children: a multi-institutional review. J Pediatr Surg. 2012 Oct;47(10):1833-6. doi: 10.1016/j.jpedsurg.2012.04.013. PubMed PMID: 23084193
4. Ladd A.P., West K.W., Rouse T.M. et al. Surgical management of duodenal injures in children // Surgery. 2002. V. 132. № 4. P. 748–753
5. Yang JC, Rivard DC, Morello FP, Ostlie DJ. Successful percutaneous drainage of duodenal hematoma after blunt trauma. J Pediatr Surg. 2008 Sep;43(9):e13-5. doi: 10.1016/j.jpedsurg.2008.03.068. PubMed PMID: 18778981
6. Dumitriu D, Menten R, Smets F, Clapuyt P. Postendoscopic duodenal hematoma in children: ultrasound diagnosis and follow-up. J Clin Ultrasound. 2014 Nov-Dec;42(9):550-3. doi: 10.1002/jcu.22145. PubMed PMID: 24615821
7. Gutierrez IM, Mooney DP. Operative blunt duodenal injury in children: a multi-institutional review. J Pediatr Surg. 2012 Oct;47(10):1833-6. doi: 10.1016/j.jpedsurg.2012.04.013. PubMed PMID: 23084193
8. Huang CL, Lee JY, Chang YT. Early laparoscopic repair for blunt duodenal perforation in an adolescent. J Pediatr Surg. 2012 May;47(5):E11-4. doi: 10.1016/j.jpedsurg.2011.12.019. PubMed PMID: 22595602
9. Mansour M.A., Moore J.B., Moore E.E., Moore F.A. Conservative management of combined pancreato duodenal injures // Am. J. Surg. 1989. V. 158. № 6. P. 531–535
10. Grigovich I.N. Rare surgical diseases of the digestive tract in children. M.: , 1985. P. 210.
11. Tsuman V.G., Scherbina V.I., Mashkov A.E. et al. Isolated damage to the retroperitoneal part of the duodenum in children // 2002. N 3. P. 4–7
12. Clendenon J.N., Meyers R.L., Nance M.L., ScaifeE.R. Management of duodenal injures in children // J. Pediatr. Surg. 2004. V. 39. № 6. P. 964–968
13. Plancq M.C., Villamizar J., Ricard J., Cana relli J.P. Management of pancreatic and duodenal injures in pediatric patients // Pediatr. Surg. Int. 2000. V. 16. №№ 1–2. P. 35–39
- Pykov M.I, Sokolov Yu.Yu., Sidneva E.A., Drozdov S.A., Logacheva T.S., Korovin S.A. Traumatic Intramural Hematoma of Duodenum in Child: a Case Report. Ultrasound and Functional Diagnostics, 2012, No.
№1, p. 78
15. Peterson ML, Abbas PI, Fallon SC, Naik-Mathuria BJ, Rodriguez JR. Management of traumatic duodenal hematomas in children. J Surg Res. 2015 Nov;199(1):126-9. doi: 10.1016/j.jss.2015.04.015. PubMed PMID: 25976857
16. Moon SB, Jung SE, Cheon JE, Kim WS, Park KW. Very large traumatic duodenal hematoma: successful percutaneous drainage in a child. Eur J Pediatr Surg. 2009 Dec;19(6):412-3. doi: 10.1055/s-0029-1202255. PubMed PMID: 19370517
Authors
Sokolov Yury Yuryevich is the head of the department of children's surgery in the Russian Medical Academy of Continuous Professional Education, doctor of medical sciences, professor, e-mail: sokolov-surg@yandex.ru
Stonogin Sergey Vasilyevich – a pediatric surgeon in the surgical unit of Government budgetary health institution Z.A. Bashlyaeva Children's Municipal Clinical Hospital of Moscow Health Department, candidate of medical sciences, e-mail: svas70@mail.ru, orcid 0000-0003-3531-5849
Tumanyan Grachik Tatevosovich - Doctor of Medical Sciences, Professor, Professor of the Department of Pediatric Surgery Russian Medical Academy of Post-Graduate Education of the Ministry of Health of the Russian Federation. 125993, Russian Federation, Moscow, Barrikadnaya St., 2/1, e-mail: tumanyan@list.ru
Allahverdiyev Israil Sadraddinovich, State budgetary institution of health care for children’s city clinical hospital of St. Vladimir, 1/3 Rubtsovsk-Palace Palace, index 107014, tel. 499-268-89-14, israil7508@mail.ru
Shapkina Anna Nikolaevna - Pacific State Medical University. Associate Professor, Department of Pediatric Surgery 690002, Russian Federation, Far Eastern Federal District, Primorsky Territory, Vladivostok, Ostryakova Avenue, Building 2.